Available services in Samar

IVF (In Vitro Fertilization)
IVF (in vitro fertilization) is a type of fertility treatment where eggs are combined with sperm outside of your body in a lab. It’s a method used by people who need help achieving pregnancy. IVF involves many complex steps and is an effective form of assisted reproductive technology (ART).
OPU surgery
Egg-retrieval technique during this procedure, an ultrasound probe is inserted into the vagina to identify follicles. A needle is guided through the vagina and into the follicles. The eggs are removed from the follicles through the needle, which is connected to a suction device.
Common complications:
-Fever, pain, bleeding, ovarian enlargement
– Ovarian cyst, ovarian hyper stimulation syndrome, Empty follicle syndrome, pelvic abscess -Pulmonary embolism, damage to the pelvic organs including intestine and urinary system
-Hematoma, emphysema, pulmonary edema, blood transfusions, shock and death
Treatment measures:
-Hospitalization, blood transfusion, hysterectomy, laparoscopy, laparotomy

Embryo transfer
There are two kinds of embryo transfers: fresh embryo transfer and frozen embryo transfer. Your healthcare provider can discuss using fresh or frozen embryos with you and decide what’s best based on your unique situation. Both frozen and fresh embryo transfers follow the same transfer process. The main difference is implied by the name.
A fresh embryo transfer means your embryo is inserted into your uterus between three and seven days after the egg retrieval procedure. This embryo hasn’t been frozen and is “fresh.”
A frozen embryo transfer means that frozen embryos (from a previous IVF cycle or donor eggs) are thawed and inserted into your uterus. This is a more common practice for logistical reasons and because this method is more likely to result in a live birth. Frozen embryo transfers can occur years after egg retrieval and fertilization.
As part of the first step in a frozen embryo transfer, you’ll take oral, injectable, vaginal or transdermal hormones to prepare your uterus for accepting an embryo. Usually, this is 14 to 21 days of oral medication followed by six days of injections. Typically, you’ll have two or three appointments during this time to monitor the readiness of your uterus with ultrasound and to measure your hormone levels with a blood test. When your uterus is ready, you’ll be scheduled for the embryo transfer procedure.
The process is similar if you’re using fresh embryos, except embryo transfer happens within three to five days of being retrieved.
The embryo transfer is a simple procedure that doesn’t require anesthesia. It feels similar to a pelvic exam or Pap smear. A speculum is placed within the vagina, and a thin catheter is inserted through the cervix into the uterus. A syringe attached to the other end of the catheter contains one or more embryos. The embryos are injected it the uterus through the catheter. The procedure typically takes less than 10 minutes.
Embryo transfer with anesthesia surgery
Common Complications:
-Infection, pain, fever, uterine injury, uterine perforation, hymen injury, intrauterine adhesion, polyp recurrence, ectopic pregnancy, multiple births, embryo transfer fraction,
Embryo transfer failure
Treatment measures:
-shock, pulmonary embolism, blood transfusion, pulmonary edema, emphysema, cervical injury
Additional comments:
A diet rich in fresh vegetables and fruits, avoiding canned food, avoiding sweets

Egg freezing surgery
Egg freezing, which is medically known as oocyte cryopreservation, is a process that is used to preserve a woman’s reproductive potential. It is an option for those women who are not ready to start a family as yet but want to ensure their ability to get pregnant at a future time. For this, eggs are harvested from the woman’s ovaries, preserved in a frozen unfertilized state, and stored for future use. When the woman decides to have a child, the frozen egg is thawed, fertilized with sperm in a lab, and then implanted in her uterus.
Common Complications:
-Fever, pain, bleeding, ovarian enlargement
– Ovarian cyst, ovarian hyper stimulation syndrome, Empty follicle syndrome, pelvic abscess -Pulmonary embolism, damage to the pelvic organs including intestine and urinary system
-Hematoma, emphysema, pulmonary edema, blood transfusions, shock and death
Treatment measures:
-Hospitalization, blood transfusion, hysterectomy, laparoscopy, laparotomy
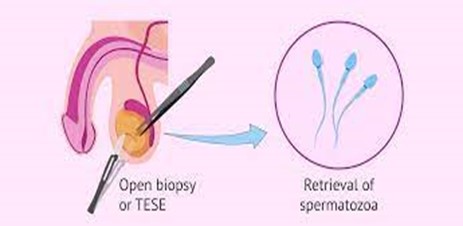
TESE surgery:
Testicular sperm extraction (TESE) involves making a small incision in the testis and examining the tubules for the presence of sperm. It is either done as a scheduled procedure or is coordinated with their female partner’s egg retrieval.
Treatment advantages:
30% to 50% sperm retrieval
Common complications:
-bleeding, infection, pain, pulmonary embolism
-shock, Testicular atrophy, fever
Treatment measures:
-Hospitalization due to infection, death, reoperation
Alternative diagnostic methods:
Embryo donation
Necessary training for patients:
-NPO till 3 hours after operation then surgical diet
-The suture is absorbable and does not require to remove. Remove the bandages 48 hours after surgery
– There is no food restriction
-Post operation visit is one week after operation
– Have a bath or shower 48 hours after surgery
-Do not have intercourse and heavy activity for one week

Hysteroscopy polypectomy / Diagnostic hysteroscopy surgery
A hysteroscopy is a procedure used to examine the inside of the womb (uterus). It’s carried out using a hysteroscope, which is a narrow telescope with a light and camera at the end. Images are sent to a monitor so your doctor or specialist nurse can see inside your womb.
Common complications:
– Infection, pain, bleeding, fever, uterine injury, uterine perforation, hymen injury, intrauterine adhesions, polyp recurrence.
Treatment measures:
– Bleeding, infection, pain, pulmonary embolism, shock, blood transfusions, hospitalization, damage to abdominal organs, death
Necessary training for patients:
– Do not have intercourse 2-3 weeks after
surgery
– Abstinence from costive and flatulent food
– taking the medications according to the prescribed instructions.
-In case of danger symptoms like; fever, pain, bleeding, infection, chest pain, dyspnea and every uncommon sign see the doctor.
-It is ordinary to have bleeding to the extent of menstruation 1-2 weeks
-Come to doctor with the pathology report
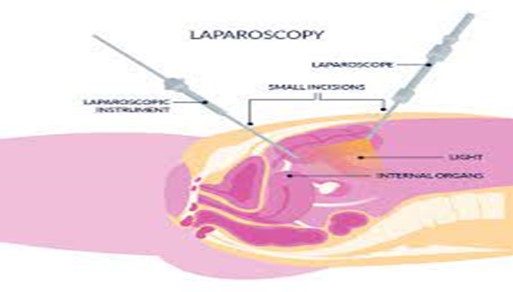
Laparoscopy surgery
What is laparoscopic surgery?
Laparoscopy is looking inside the abdomen with a telescope. This procedure is used to make a diagnosis but also to carry out several surgical procedures and the common name used for this technique is laparoscopic or key-hole surgery. It is also known as minimal access surgery.
What are the common indications?
In gynecology, common indications for performing laparoscopic surgery are:
- Endometriosis(diagnosis and treatment)
- Ovarian cysts(cystectomy is often performed laparoscopically)
- Fibroids(myomectomy)
- Ectopic pregnancy (diagnosis and treatment)
- Hysterectomy (may be performed for heavy periods, fibroidsor endometrial cancer)
- Diagnosis and treatment of pelvic pain
How common is laparoscopic surgery?
Laparoscopic approach is now the default way of performing many standard operations including major procedures such as hysterectomy and myomectomy. Open surgery has now become relatively uncommon.
How is laparoscopic surgery performed?
Under general anesthesia, a small 5mm incision is made inside the umbilicus and a needle is inserted to inflate the abdominal cavity with gas. This is necessary to provide adequate space to perform the procedure safely. A telescope (long tube with camera at one end) is then inserted inside the abdomen. The image is displayed on a television screen and all surgery is carried out under direct vision. This can be recorded in the form of pictures and video.
Two or three further incisions are made (5-10 mm) to insert various instruments so that surgery can be carried out. This is often likened to painting a hallway through a letterbox! This is a complex skill acquired through many hours of practice and simulation training.
Common Complications:
-Pain, bleeding, fever due to infection, abscess, pulmonary embolism, complications due to anesthesia (sore throat, nausea and vomiting…), pelvic and abdominal wall adhesion, urination disorders, hospitalization, blood transfusion, reoperation, death
– Diminished ovarian reserve, early menopause, infertility, colostomy, fistula
– Damage to the pelvic organs including intestine, urinary system, fallopian tubes And ovaries
– Depending on the reason for the surgery it will be done; hysterectomy (remove the womb) and salpingectomy (remove the fallopian tubes), oophorectomy (remove the ovaries) and partial colectomy (remove the colon) or partial cystectomy (remove the bladder) at the doctor’s discretion
Necessary training for patients:
-Do not have intercourse till doctor’s permission
– Abstinence from costive and flatulent food
-Take clear liquids later the same day
-Walking
-Come to doctor to take bandages off
-Come to doctor with the pathology report
-In case of danger symptoms like; fever, pain, bleeding, infection, chest pain, dyspnea and every uncommon sign, see the doctor.
Hemovac Drain Care:

The hemovac drain removes fluid by creating suction in the tube. The circular device is squeezed flat. The device expands as it fills with fluid.
-Empty the drain when it is half full or every 4 to 8 hours: wash your hands with soap and water, remove the plug from the top of the drain, pour the fluid into a measuring cup, clean the plug with an alcohol swab or a cotton ball dipped in rubbing alcohol, squeeze the drain flat and put the plug back in. The drain should stay flat until it starts to fill with fluid again, make sure the tubing is not kinked or twisted. Refasten to your clothes below your surgery site so it does not pull at your skin, measure the amount of fluid you pour out. Write down how much fluid you empty from the drain and the date and time you collected it. Bring this record with you to your follow-up visits, flush the fluid down the toilet. Wash your hands. The amount of fluid that you drain should decrease each day. Ask your healthcare provider when and how your drain will be removed.
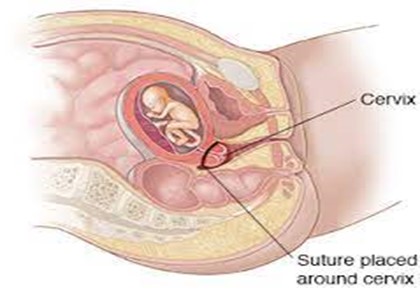
Cerclage surgery
A cervical cerclage is a treatment that involves temporarily sewing the cervix closed with stitches. This may help the cervix hold a pregnancy in the uterus. A cerclage is done in the second trimester of pregnancy to prevent preterm birth.
Common Complications:
-Infection, pain, bleeding, fever, damage to pelvic organs (urinary system and blood vessel) Hematoma, emphysema, pulmonary edema, damage to cervix, blood transfusions, premature rupture of membranes (Amniotic sac), abortion, hospitalization, preterm labor, shock and death
Treatment advantages:
Cervical cerclage helps prevent miscarriage or premature labor caused by cervical incompetence.
Necessary training for patients:
– Do not have intercourse till doctor’s permission
– Abstinence from costive and flatulent food
– taking the medications according to the prescribed instructions.
-In case of danger symptoms like; fever, pain, bleeding, infection, chest pain, dyspnea and every uncommon sign see the doctor.
-Relative bed rest
-See doctor 24 till 48 hours after surgery in order to carry out sonographic estimation of amniotic fluid volume.
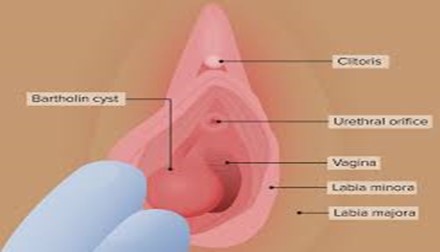
Surgical drainage Bartholin’s cyst:
The Bartholin glands lie at the entrance to the vagina. They produce fluid which lubricates the vagina through a small duct in each gland. A cyst may form if the duct becomes blocked and if the cyst becomes infected an abscess may form. Approximately one in every 50 women develops a Bartholin’s cyst or abscess. It can affect anyone, though it is more common in sexually active women at child-bearing age. In most cases the cause is unknown and there is little that can be done to prevent it.
Marsupialization: During this procedure, a small cut is made in the abscess and gland to allow the fluid to drain and then sewing the edges of the surrounding skin. This allows the incision to stay open so it can heal and the contents of the abscess can continue to drain. This helps to prevent another abscess from forming later as it allows for normal secretions from Bartholin’s gland to drain. This cut will heal by itself eventually. A sample of the tissue may be sent to pathology for examination. If so, the results will be sent to you. This usually takes 3 – 4 weeks.
Common Complications:
-Infection, pain, bleeding, shock, pulmonary embolism, pulmonary edema, emphysema, blood transfusion, hospitalization, death
Necessary training for patients:
-personal cleanliness
-Do not have intercourse till one month after
surgery
-Avoiding exercises such as swimming during one month after surgery
– Abstinence from costive and flatulent food
– Taking antibiotics according to the prescribed instructions.
Following your surgery
Stitches will be dissolvable and do not need to be removed.
- You may have a quick bath / shower after 24 hours, thereafter daily. Plain water is best. Do not rub the wound dry, pat dry or use a hairdryer.
- Dressings: you may have some gauze swabs over the wound and a pad for your underwear. It is advisable to wear soft pads while healing is taking place.
- There may be some blood loss from the wound. If the wound bleeds heavily put the gauze swabs over the wound and press for five minutes. This should stop the bleeding.
- You may experience some mild to moderate pain which can be relieved by taking Page 2 of 2 painkillers such as paracetamol and ibuprofen or other similar pain-relieving medication.
- To reduce the risk of infection, please use sanitary towels or panty liners not tampons until your next period. These should be changed regularly.
- Do not have sexual intercourse for 2 weeks to allow healing to take place.
- It is quite normal for the operation site to feel sensitive and bruising to be present.
Anterior and posterior vaginal wall repair surgery:
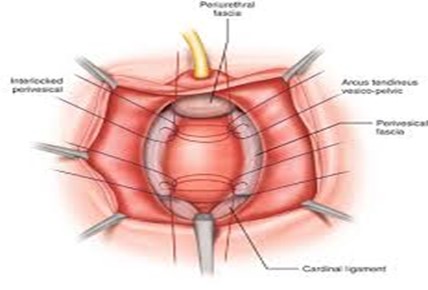
Anterior and posterior repair are minimally invasive procedures used to correct pelvic organs that have dropped out of their normal positions.
When the tissues that support the pelvic organs become weak, stretched or damaged, due to age or childbirth for example, the organs can slip out of place, dropping down and pressing against the walls of the vagina. This is known as pelvic organ prolapse. These sagging organs create a bulge in the vagina, causing pressure, pain, discomfort, and urinary and bowel dysfunction, among other symptoms.
Anterior and posterior repair are used to tighten the support tissues that hold these organs in place, restoring their normal position and function.
Anterior repair is used to tighten the front (anterior) wall of the vagina. It is used when the bladder drops out of its normal position and bulges into the front of the vagina, causing the front wall of the vagina to sag. This condition is known as anterior wall prolapse, cystocele or dropped bladder. During the surgery, the bladder is pushed back into its normal position and the support tissue between the front of the vagina and the bladder is tightened and reinforced. The procedure is also called an anterior vaginal wall repair or anterior colporrhaphy.
Posterior repair is used to tighten the back (posterior) wall of the vagina. It is used when the rectum drops out of its normal position and bulges into the back of the vagina, causing the back wall of the vagina to sag, which may result in bowel dysfunction. This condition is known as posterior wall prolapse, rectocele or fallen rectum. During the surgery the rectum is pushed back into to its normal position, and the support tissue between the back of the vagina and the rectum is tightened and reinforced. The procedure is also called a posterior vaginal wall repair or posterior colporrhaphy.
Common Complications:
-Infection, pain, bleeding, hematoma, abscess, damage to urinary system and pelvic organs, emphysema, pulmonary embolism, complications due to anesthesia (sore throat, nausea and vomiting…), pelvic and abdominal wall adhesion, urination disorders, hospitalization, relapse, blood transfusion, reoperation, death
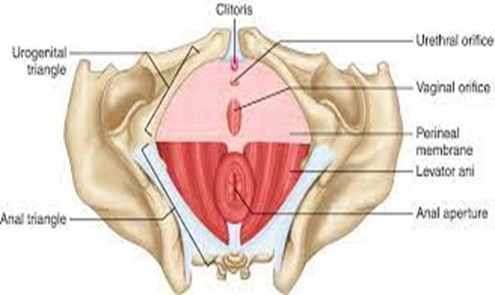
Labiaplasty and Perineoplasty surgery:
The area between the vagina and the rectum is called the perineum. Perineoplasty is a procedure of reconstructing the vaginal opening in order to repair damage to the perineum and/or damage to the vulva which can be caused by child birth, intercourse, obesity, or inadequate innervation. Perineoplasty can be performed for medical or cosmetic reasons.
The term labiaplasty refers to a procedure that reduces the length of the labia minora. It is the most commonly performed vaginal rejuvenation procedure and it can relieve symptoms women experience from twisting and tugging of the labia.
Common Complications:
-Infection, pain, bleeding, fever, abscess, hematoma, damage to urinary system and pelvic organs, emphysema, pulmonary embolism, pulmonary edema, shock, blood transfusion, relapse,
Hospitalization, dissymmetry between the lips, reoperation, proud flesh, stiches, suture
dehiscence.
